*/

On 23 June 2025 the Department of Health and Social Care (DHSC) announced a rapid national investigation into maternity and neonatal services to be led by Baroness Valerie Amos. The purpose of this investigation is ‘to provide truth and accountability for families harmed’ and ‘to drive urgent improvements in care and safety’. Is this what is needed to effect change after the near constant scrutiny over the past decade? Why have the Mid Staffordshire public inquiry, Morecambe Bay investigation, Shrewsbury and Telford review, East Kent investigation and the Nottingham review not been enough? Why, after so much time and so much investigation, are maternity services still failing?
Successive inquiries have laid bare a pattern of preventable harm in a system paralysed with inadequate staffing, poor communication and a reluctance to learn from past mistakes. In 2013, Robert Francis KC, following his public inquiry into the failings at the Mid Staffordshire Trust, wrote that: ‘the story it tells is first and foremost of appalling suffering of many patients… A culture focused on doing the system’s business – not that of the patients… An institutional culture which ascribed more weight to positive information about the service than to information capable of implying cause for concern… Too great a degree of tolerance of poor standards and of risk to patients… A failure to appreciate until recently the risk of disruptive loss of corporate memory and focus resulting from repeated, multi-level reorganisation.’
With the Shrewsbury review examining over 1,500 cases and the Nottingham review approximately 2,500 cases, why are we still there?
A case we were recently involved in sets out just how little progress has been made. Ida died in late 2019 but through obfuscation and delays largely on the part of the Trust, we did not resume the inquest until February 2025. By that point, there were more than 30,000 pages of disclosure which revealed systemic failings across the Trust, including the governance process.
It is important to recognise that the NHS, when it works, is a truly remarkable thing. For many, it has been the difference between life and death. It must also be recognised that there are restrictions on resources and expertise and that many clinicians, despite these difficulties provide exceptional care to those in need. However, Ida did not receive the care or treatment that she deserved and neither did her parents. Ida was failed in many ways, but some examples include:
Ida’s family had never wanted to involve lawyers. They did not want litigation. They simply wanted to understand how their daughter had come to die. Why did it take years of questions and a lengthy inquest to uncover that? All healthcare professionals have a duty of candour; a professional responsibility to be honest when things go wrong, it is enshrined in their regulatory bodies’ code of conduct and a statutory duty of candour. The NHS Resolution Saying Sorry guidance (2023) sets out: ‘Not only is it a moral and right thing to do – it is also a statutory, regulatory, and professional requirement. It can also support learning and improve patient safety.’
It is not, however, enough to simply write it down. It must be put into action. In Ida’s case, the Trust was confrontational and obstructive. Despite a thorough and detailed report from the Healthcare Safety Investigation Branch (HSIB, now Maternity and Newborn Safety Investigations (MNSI)) the Trust instructed independent medico legal experts to comment on its case. The Trust subsequently refused to disclose those reports which, the coroner recorded, ‘produced the somewhat surreal situation where the Department of Health, through its arm’s length organisation NHS Resolutions, was obtaining expert reports to disagree with the Secretary of State for Health’s independent panel of experts at the HSIB’.
Dr Bill Kirkup CBE, Chair of the Morecambe Bay Investigation in 2015, concluded that the 2020 root cause analysis (RCA) report in Ida’s case showed nearly all the same features as identified in his 2015 report. Some of the issues highlighted in the 2015 report were that ‘investigations were flawed, relying upon poor-quality records that conflicted with patients’ and relatives’ accounts’. Dr Kirkup said that the RCA was – as he had found in the cases he considered in 2015 – superficial, protective, brief and failed to identify problems.
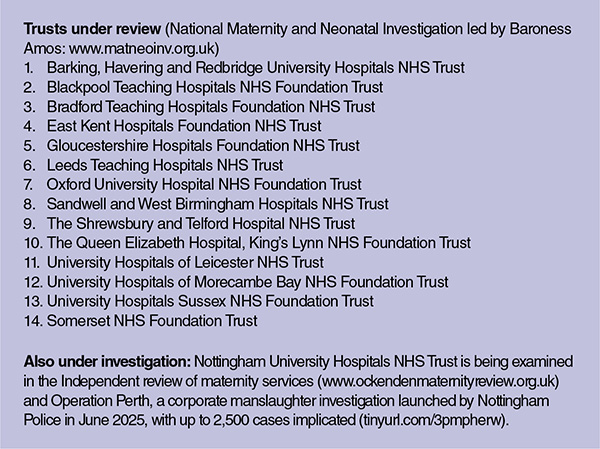
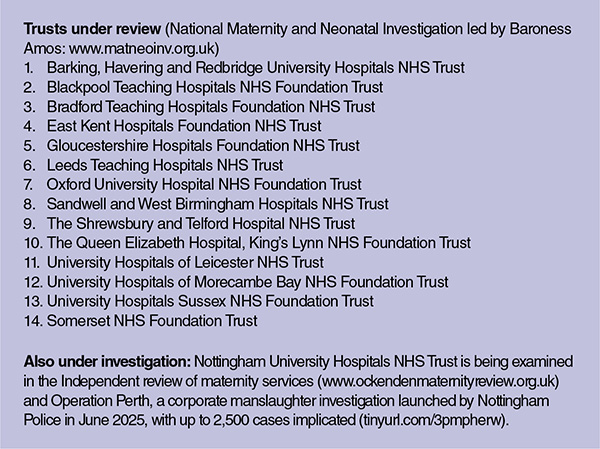
A beacon of light in Ida’s case was the investigator at the MNSI. An objective investigator, who met with the family and the clinicians involved, interrogated the records and reached fair and balanced conclusions without blame of individuals but rather providing a holistic system assessment. This independent oversight enabled clear identification of problems with care and areas of learning; something the Trust chose to challenge and argue against. Further evidence that mistakes continue to be concealed or rationalised rather than openly investigated. That same Trust which had advocated that it had complied with Dr Kirkup’s recommendations finds itself on the list to be investigated by Baroness Amos (see box).
More has to be done; assurances from hospitals and Trusts that they have ‘learnt’ and will ‘improve’ are not reliable. In short, they cannot mark their own homework; independent, specialist oversight is required and accountability is mandated. Learning from failure should be seen as a marker of strength and not weakness.
In December 2025, Baroness Amos published an update (Reflections and Initial Impressions). It is clear that she, too, cannot comprehend why recommendations are not acted upon, describing how she ‘could not understand why, having read the media reports over the years of the experiences of harmed and bereaved families, so little seemed to have changed and why families continued to go through such trauma and distress.
‘I expected to hear experiences from families about where they had been let down by the care they had received in maternity and neonatal units across the country, but nothing prepared me for the scale of unacceptable care that women and families have received, and continue to receive, the tragic consequences for their babies, and the impact on their mental, physical and emotional wellbeing.’
Baroness Amos identifies ‘a staggering 748 recommendations relating to maternity and neonatal care, the majority of which have been made since 2015, and other organisations have also made recommendations. This naturally raises an important question: with so many thorough and far-reaching reviews already completed, why are we in England still struggling to provide safe, reliable maternity and neonatal care everywhere in the country?’ Next steps on the review include a call for evidence and the completion of site visits.
Tommy’s helpline 0800 0147 800; email midwife@tommys.org; www.tommys.org/baby-loss-support
Sands helpline 0808 164 3332; email helpline@sands.org.uk; www.sands.org.uk/support-you

On 23 June 2025 the Department of Health and Social Care (DHSC) announced a rapid national investigation into maternity and neonatal services to be led by Baroness Valerie Amos. The purpose of this investigation is ‘to provide truth and accountability for families harmed’ and ‘to drive urgent improvements in care and safety’. Is this what is needed to effect change after the near constant scrutiny over the past decade? Why have the Mid Staffordshire public inquiry, Morecambe Bay investigation, Shrewsbury and Telford review, East Kent investigation and the Nottingham review not been enough? Why, after so much time and so much investigation, are maternity services still failing?
Successive inquiries have laid bare a pattern of preventable harm in a system paralysed with inadequate staffing, poor communication and a reluctance to learn from past mistakes. In 2013, Robert Francis KC, following his public inquiry into the failings at the Mid Staffordshire Trust, wrote that: ‘the story it tells is first and foremost of appalling suffering of many patients… A culture focused on doing the system’s business – not that of the patients… An institutional culture which ascribed more weight to positive information about the service than to information capable of implying cause for concern… Too great a degree of tolerance of poor standards and of risk to patients… A failure to appreciate until recently the risk of disruptive loss of corporate memory and focus resulting from repeated, multi-level reorganisation.’
With the Shrewsbury review examining over 1,500 cases and the Nottingham review approximately 2,500 cases, why are we still there?
A case we were recently involved in sets out just how little progress has been made. Ida died in late 2019 but through obfuscation and delays largely on the part of the Trust, we did not resume the inquest until February 2025. By that point, there were more than 30,000 pages of disclosure which revealed systemic failings across the Trust, including the governance process.
It is important to recognise that the NHS, when it works, is a truly remarkable thing. For many, it has been the difference between life and death. It must also be recognised that there are restrictions on resources and expertise and that many clinicians, despite these difficulties provide exceptional care to those in need. However, Ida did not receive the care or treatment that she deserved and neither did her parents. Ida was failed in many ways, but some examples include:
Ida’s family had never wanted to involve lawyers. They did not want litigation. They simply wanted to understand how their daughter had come to die. Why did it take years of questions and a lengthy inquest to uncover that? All healthcare professionals have a duty of candour; a professional responsibility to be honest when things go wrong, it is enshrined in their regulatory bodies’ code of conduct and a statutory duty of candour. The NHS Resolution Saying Sorry guidance (2023) sets out: ‘Not only is it a moral and right thing to do – it is also a statutory, regulatory, and professional requirement. It can also support learning and improve patient safety.’
It is not, however, enough to simply write it down. It must be put into action. In Ida’s case, the Trust was confrontational and obstructive. Despite a thorough and detailed report from the Healthcare Safety Investigation Branch (HSIB, now Maternity and Newborn Safety Investigations (MNSI)) the Trust instructed independent medico legal experts to comment on its case. The Trust subsequently refused to disclose those reports which, the coroner recorded, ‘produced the somewhat surreal situation where the Department of Health, through its arm’s length organisation NHS Resolutions, was obtaining expert reports to disagree with the Secretary of State for Health’s independent panel of experts at the HSIB’.
Dr Bill Kirkup CBE, Chair of the Morecambe Bay Investigation in 2015, concluded that the 2020 root cause analysis (RCA) report in Ida’s case showed nearly all the same features as identified in his 2015 report. Some of the issues highlighted in the 2015 report were that ‘investigations were flawed, relying upon poor-quality records that conflicted with patients’ and relatives’ accounts’. Dr Kirkup said that the RCA was – as he had found in the cases he considered in 2015 – superficial, protective, brief and failed to identify problems.
A beacon of light in Ida’s case was the investigator at the MNSI. An objective investigator, who met with the family and the clinicians involved, interrogated the records and reached fair and balanced conclusions without blame of individuals but rather providing a holistic system assessment. This independent oversight enabled clear identification of problems with care and areas of learning; something the Trust chose to challenge and argue against. Further evidence that mistakes continue to be concealed or rationalised rather than openly investigated. That same Trust which had advocated that it had complied with Dr Kirkup’s recommendations finds itself on the list to be investigated by Baroness Amos (see box).
More has to be done; assurances from hospitals and Trusts that they have ‘learnt’ and will ‘improve’ are not reliable. In short, they cannot mark their own homework; independent, specialist oversight is required and accountability is mandated. Learning from failure should be seen as a marker of strength and not weakness.
In December 2025, Baroness Amos published an update (Reflections and Initial Impressions). It is clear that she, too, cannot comprehend why recommendations are not acted upon, describing how she ‘could not understand why, having read the media reports over the years of the experiences of harmed and bereaved families, so little seemed to have changed and why families continued to go through such trauma and distress.
‘I expected to hear experiences from families about where they had been let down by the care they had received in maternity and neonatal units across the country, but nothing prepared me for the scale of unacceptable care that women and families have received, and continue to receive, the tragic consequences for their babies, and the impact on their mental, physical and emotional wellbeing.’
Baroness Amos identifies ‘a staggering 748 recommendations relating to maternity and neonatal care, the majority of which have been made since 2015, and other organisations have also made recommendations. This naturally raises an important question: with so many thorough and far-reaching reviews already completed, why are we in England still struggling to provide safe, reliable maternity and neonatal care everywhere in the country?’ Next steps on the review include a call for evidence and the completion of site visits.
Tommy’s helpline 0800 0147 800; email midwife@tommys.org; www.tommys.org/baby-loss-support
Sands helpline 0808 164 3332; email helpline@sands.org.uk; www.sands.org.uk/support-you


The Bar Council is ready to support a turn to the efficiencies that will make a difference
By Louise Crush of Westgate Wealth Management
Marie Law, Director of Toxicology at AlphaBiolabs, examines the latest ONS data on drug misuse and its implications for toxicology testing in family law cases
An interview with Rob Wagg, CEO of New Park Court Chambers
What meaningful steps can you take in 2026 to advance your legal career? asks Thomas Cowan of St Pauls Chambers
Marie Law, Director of Toxicology at AlphaBiolabs, explains why drugs may appear in test results, despite the donor denying use of them
Ever wondered what a pupillage is like at the CPS? This Q and A provides an insight into the training, experience and next steps
The appointments of 96 new King’s Counsel (also known as silk) are announced today
Ready for the new way to do tax returns? David Southern KC continues his series explaining the impact on barristers. In part 2, a worked example shows the specific practicalities of adapting to the new system
Resolution of the criminal justice crisis does not lie in reheating old ideas that have been roundly rejected before, say Ed Vickers KC, Faras Baloch and Katie Bacon
With pupillage application season under way, Laura Wright reflects on her route to ‘tech barrister’ and offers advice for those aiming at a career at the Bar